Connect With Us

Stretching Your Feet May Prevent Foot Injuries
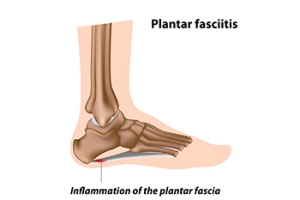
 Physical activities like running and jogging are great ways to stay in shape, however, vigorous exercise can also potentially lead to injuries of the plantar fascia, a thick band of tissue that runs along the bottom of your feet. When the plantar fascia is put under too much stress, it can tear and become inflamed, leading to plantar fasciitis. This condition may cause pain and reduced flexibility in your feet. To reduce the risk of developing plantar fasciitis, it is suggested that you stretch your feet regularly. For a gentle stretch, sit on a chair and bend your right leg to place your right ankle on your left knee. Hold your right toes, gently pressing them into a pointed position, and hold there for a few seconds. Then hold your right toes and gently pull them backwards, flexing your foot, and hold for a few seconds. Repeat this several times with each foot. For more information on what you can do to decrease your risk of developing plantar fasciitis, consult with a podiatrist.
Physical activities like running and jogging are great ways to stay in shape, however, vigorous exercise can also potentially lead to injuries of the plantar fascia, a thick band of tissue that runs along the bottom of your feet. When the plantar fascia is put under too much stress, it can tear and become inflamed, leading to plantar fasciitis. This condition may cause pain and reduced flexibility in your feet. To reduce the risk of developing plantar fasciitis, it is suggested that you stretch your feet regularly. For a gentle stretch, sit on a chair and bend your right leg to place your right ankle on your left knee. Hold your right toes, gently pressing them into a pointed position, and hold there for a few seconds. Then hold your right toes and gently pull them backwards, flexing your foot, and hold for a few seconds. Repeat this several times with each foot. For more information on what you can do to decrease your risk of developing plantar fasciitis, consult with a podiatrist.
Stretching the feet is a great way to prevent injuries. If you have any concerns with your feet consult with Dr. Michael D. Garvin from Florida. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Stretching the Feet
Being the backbone of the body, the feet carry your entire weight and can easily become overexerted, causing cramps and pain. As with any body part, stretching your feet can serve many benefits. From increasing flexibility to even providing some pain relief, be sure to give your feet a stretch from time to time. This is especially important for athletes or anyone performing aerobic exercises, but anyone experiencing foot pain or is on their feet constantly should also engage in this practice.
Great ways to stretch your feet:
- Crossing one leg over the others and carefully pull your toes back. Do 10-20 repetitions and repeat the process for each foot
- Face a wall with your arms out and hands flat against the wall. Step back with one foot and keep it flat on the floor while moving the other leg forward. Lean towards the wall until you feel a stretch. Hold for 30 seconds and perform 10 repetitions for each foot
- Be sure not to overextend or push your limbs too hard or you could risk pulling or straining your muscle
Individuals who tend to their feet by regular stretching every day should be able to minimize foot pain and prevent new problems from arising.
If you have any questions, please feel free to contact our offices located in Port St. Lucie, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Stretching Your Feet
Debilitating foot pain is a problem for many people. But just as stretching the torso can help alleviate back pain, stretching the feet can also help mend existing foot problems and prevent future ones.
The feet, as the body’s foundation, carry the body’s entire weight and can get easily strained from overexertion. Persistent sharp pain and cramping in the feet are often common concerns. Foot pain and foot problems can be due to any number of causes, and in many cases pain may be eased without medication or doctor visits. It is always a good idea, however, to first rule out any serious medical issues with a physician.
Stretching can help relax the feet and alleviate pain, but is especially important before heavy aerobic exercise. Stretching before such activities can help you avoid experiencing painful cramps or strained foot muscles. Stretches should be performed slowly and deliberately without forceful pulling. The stretch should be held for several seconds before relaxing.
A great way to stretch out and loosen up the foot muscles while sitting is to cross one leg over the other and pull the toes carefully back without overextending. Start by resting the left ankle on the right knee. With the left hand, gently flex the left foot by pulling back on the toes. Do not pull too hard; just hard enough to feel the stretch in the arch of the foot. Then point the toes of the left foot as far as you can. Rotate the motion of pointing with pulling back on the toes. This should relax and stretch the muscles on the bottom and the top of the foot. Doing this stretch ten to twenty times should bring relief. Repeat the whole process for the other foot by resting the right ankle on the left knee.
A stretch that focuses on the often injured Achilles tendon involves standing and facing a wall with your arms out and hands flat against the wall. Step back with one foot, keeping it flat against the floor. Move the other leg forward and lean toward the wall. You should feel a stretch through the back of your leg and your Achilles tendon, but do not push yourself too much. Stop when you feel a stretching sensation, and hold for 30 seconds. Ten repetitions may be done for each foot.
Stretching the feet is important for athletes or those performing aerobic exercise, but it can also help anyone with foot pain caused by poor footwear, plantar fasciitis, or long hours standing and walking. Individuals who tend to their feet by regularly stretching every day should be able to minimize foot pain and prevent new problems from arising.
Common Foot and Toe Injuries

The feet, ankles, and toes are intricate structures that bear the brunt of your daily activities. Unfortunately, injuries in these areas are not uncommon and can be quite painful. Ankle sprains often occur due to missteps or awkward landings, causing ligaments to stretch or tear. Stress fractures in the feet, often seen in runners, result from repetitive impact on the bones. Additionally, Achilles tendonitis can afflict the back of the ankle, causing pain and inflammation. Toes are not exempt, as stubbing or jamming them can lead to fractures or dislocations. Relief may come from getting adequate rest, and using compression and elevation may help to reduce existing swelling. For more severe injuries, seeking medical attention is essential for proper healing and to prevent long-term issues. Wearing proper footwear, performing warm up exercises, and being mindful of your surroundings can also reduce the risk of these injuries, allowing you to keep moving comfortably. If you have injured your foot, toe or ankle, it is strongly suggested that you consult a podiatrist who can effectively treat these types of foot conditions.
Foot and ankle trauma is common among athletes and the elderly. If you have concerns that you may have experienced trauma to the foot and ankle, consult with Dr. Michael D. Garvin from Florida. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Foot and ankle trauma cover a range of injuries all over the foot; common injuries include:
- Broken bones
- Muscle strains
- Injuries to the tendons and ligaments
- Stress fractures
Symptoms
Symptoms of foot and ankle injuries vary depending on the injury, but more common ones include:
- Bruising
- Inflammation/ Swelling
- Pain
Diagnosis
To properly diagnose the exact type of injury, podiatrists will conduct a number of different tests. Some of these include sensation and visual tests, X-rays, and MRIs. Medical and family histories will also be taken into account.
Treatment
Once the injury has been diagnosed, the podiatrist can than offer the best treatment options for you. In less severe cases, rest and keeping pressure off the foot may be all that’s necessary. Orthotics, such as a specially made shoes, or immobilization devices, like splints or casts, may be deemed necessary. Finally, if the injury is severe enough, surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Port St. Lucie, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot and Ankle Fractures
When the foot or ankle experiences trauma, a fracture may occur. Causes of foot and ankle fractures can vary; in some cases, an obvious impact to the foot or a fall can be behind a fracture. Alternatively, fractures can also occur because of increased stress on the bone over time. The location of the fracture can often give your podiatrist information on how the fracture occurred.
Pain, especially when bearing weight, is a telltale sign of a fracture. Limping due to this pain is a further sign of a foot or ankle fracture. Other symptoms include inflammation, bruising, deformity, and tenderness. A deformity may occur due to a shift in bone alignment or a joint dislocation near the fracture. While pain is a significant symptom of breakage, a patient who has nerve damage or who has diabetes may not feel this pain. In this instance, your podiatrist will look for additional signs to determine whether a fracture has occurred.
If you are experiencing severe pain, cannot walk without limping, have an open wound near the suspected break, or have numbness or tingling in the toes, you should see your podiatrist.
A Guide to Treating Plantar Fasciitis

Plantar fasciitis, a common and often debilitating foot condition, can bring your daily life to a halt due to severe heel pain. Fortunately, various treatment options are available to help you regain your comfort and mobility. Conservative measures like rest and taking anti-inflammatory medications can help to alleviate discomfort. Wearing supportive footwear with proper arch support and cushioning can significantly reduce strain on the plantar fascia. Stretching exercises that target the calf muscles and Achilles tendon can also provide relief by loosening tight structures around the foot. Custom orthotics may be recommended to support the arch and distribute pressure evenly. In rare cases, when conservative treatments are not sufficient, medical interventions such as cortico-steroid injections or surgery may be considered. Plantar fasciitis can be challenging, but with the right approach and patience, you can overcome it and return to a pain-free, active lifestyle. If you have heel pain, it is suggested that you contact a podiatrist who can effectively diagnose and treat plantar fasciitis.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Michael D. Garvin from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our offices located in Port St. Lucie, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Footwear Influence on Bunions

Bunions, or hallux valgus, is a foot deformity where the big toe tilts toward the second toe, causing a bony lump on the side of the foot. Symptoms include pain, swelling, callused skin, and changes in foot shape. Contrary to popular belief, fashion shoes such as high heels do not directly cause bunions. Bunions are primarily the result of a genetic predisposition and the mechanical structure of the foot. However, wearing shoes that squeeze the forefoot and crowd the toes can worsen an existing condition and lead to pain and joint deformity. Bunions can also develop due to factors such as age, arthritis, or sports activities. Preventing bunions involves choosing sensible, well fitting footwear with ample toe room. Avoiding pointed shoes and excessive heels can be helpful. Proper footwear, non surgical treatments and wearing orthotics are initial choices. Surgery is typically the last option for bunions causing significant pain. This involves removing the bony lump and realigning the big toe, ultimately improving foot function and comfort. If you have a bunion that is causing discomfort, it is suggested that you make an appointment with a podiatrist to have it evaluated and obtain appropriate treatment.
If you are suffering from bunion pain, contact Dr. Michael D. Garvin of Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Port St. Lucie, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is an enlargement of the base joint of the toe that connects to the foot, often formed from a bony growth or a patch of swollen tissues. It is caused by the inward shifting of the bones in the big toe, toward the other toes of the foot. This shift can cause a serious amount of pain and discomfort. The area around the big toe can become inflamed, red, and painful.
Bunions are most commonly formed in people who are already genetically predisposed to them or other kinds of bone displacements. Existing bunions can be worsened by wearing improperly fitting shoes. Trying to cram your feet into high heels or running or walking in a way that causes too much stress on the feet can exacerbate bunion development. High heels not only push the big toe inward, but shift one's body weight and center of gravity towards the edge of the feet and toes, expediting bone displacement.
A podiatrist knowledgeable in foot structure and biomechanics will be able to quickly diagnose bunions. Bunions must be distinguished from gout or arthritic conditions, so blood tests may be necessary. The podiatrist may order a radiological exam to provide an image of the bone structure. If the x-ray demonstrates an enlargement of the joint near the base of the toe and a shifting toward the smaller toes, this is indicative of a bunion.
Wearing wider shoes can reduce pressure on the bunion and minimize pain, and high heeled shoes should be eliminated for a period of time. This may be enough to eliminate the pain associated with bunions; however, if pain persists, anti-inflammatory drugs may be prescribed. Severe pain may require an injection of steroids near the bunion. Orthotics for shoes may be prescribed which, by altering the pressure on the foot, can be helpful in reducing pain. These do not correct the problem; but by eliminating the pain, they can provide relief.
For cases that do not respond to these methods of treatment, surgery can be done to reposition the toe. A surgeon may do this by taking out a section of bone or by rearranging the ligaments and tendons in the toe to help keep it properly aligned. It may be necessary even after surgery to wear more comfortable shoes that avoid placing pressure on the toe, as the big toe may move back to its former orientation toward the smaller toes.
Causes and Risk Factors of Foot Stress Fractures

Stress fractures are microscopic cracks in bones, and can significantly impact foot health and mobility. These fractures are often the result of repetitive strain and overuse, which can gradually weaken the bones. Athletes, especially runners and dancers, are susceptible to developing a foot stress fracture, as a result of the constant impact on their feet. Sudden increases in activity intensity or duration can also trigger stress fractures. Factors such as wearing improper footwear, inadequate rest between activities, and poor foot structure can lead to a heightened risk of incurring a stress fracture. Additionally, medical conditions such as osteoporosis can reduce bone density, and increase vulnerability. Individuals with certain nutritional deficiencies, hormonal imbalances, or a history of stress fractures can face an elevated risk. Preventative measures include proper training progression, adequate nutrition, and wearing supportive shoes. If you have a foot stress fracture, it is suggested that you confer with a podiatrist who can effectively treat this condition.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact Dr. Michael D. Garvin from Florida. Our doctor can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact our offices located in Port St. Lucie, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.